Nodular Prurigo: A case study
June 30, 2020Fever, Loss Of Smell And Severe Cough: A Case Study
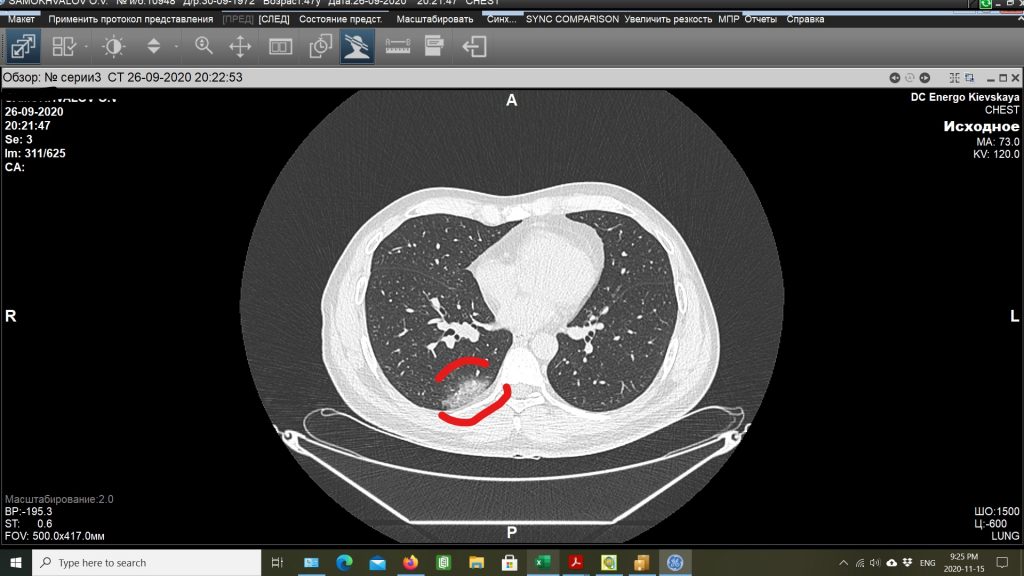
April 26, 2021A case study: A 48-year-old male travelled to St. Petersburg, Russia, to visit his family. On September 25th, 2020 he developed a fever of 39.4 degrees Celsius accompanied by a minor cough, severe chills, and shivering. He visited a local diagnostic center, and a CT scan was performed. The CT scan reveals “ground-glass-like subpleural interstitial infiltration located in the right lower segment of the Lung”. The infiltration margin was 2.6 x 5.1 centimetres. The etiology most likely correlates to viral pneumonia. It was recommended that the patient visit a doctor. Upon consultation with the doctor over the phone, the patient was diagnosed with viral pneumonia and suspected COVID-19 infection. The patient was prescribed chloramphenicol (Levomecitin) to prevent further complications. After the first dosage, the patient developed an adverse drug reaction in the form of a severe skin rash. Thus, the patient decided to try Traditional Chinese Medicine. On September 26th, he had a consultation online with me. His tongue body was swollen and slightly red with a greasy thick coating on both sides. The patient presented with a chief complaint of severe chills accompanied by shivering, a fever of 39.4 degrees Celsius, and a mild cough. He reported no shortness of breath but stated a prevalence of exhaustion and severe fatigue.

Case analysis:
On December 31, 2019, China reported cases of unexplained atypical pneumonia in the province of Wuhan, Hubei. It was found later that the cause for the epidemy is a new virus strain that belongs to the group of coronaviruses. The National Health Commission of the People’s Republic of China and the National Administration of Traditional Chinese Medicine of the People’s Republic of China officially included TCM in the treatment and diagnosis of COVID-19 pneumonia1. Furthermore, this was only a suspected case. A PCR (Polymerase chain reaction) test was not performed due to different circumstances. I decided to take the damp-toxin approach, as described in “The Lantern” – Journal of Chinese Medicine by Dr. Jin Zhao and Chris Flanagan2. In Wu Youke’s article, “Discussion of Warm Epidemics”, at the onset of a warm epidemic, first there is an increased sense of cold and after there is a fever.” “The warm-epidemic tongue has a white coating; this is because the pathogen is at the “mo yuan” (membrane source1)” 2.
The treatment strategy: disperse damp-toxin from “Mo Yuan” (Membrane Source – interstitial space), Disperse Lungs, and eliminate Phlegm2.
According to Dr. Jin Zhao, the treatment should be based on a combination of Huo Po Xia Ling Tang and Da Mo Yuan Yin Modifications, with the most important herbs including: Ban Xia Pinelliae Rhizoma praeparatum, Huo Xiang (Pogostemonis/ Agastaches Herba), Hou Po (Magnoliae officinalis Cortex), Bai Dou Kou (Amomi Fructus rotundus), Bing Lang (Arecae Semen), and Cao Guo (Tsaoko Fructus)2. Since the patient’s tongue is slightly red in color, this indicates a blood-toxin is present at the blood level. Therefore, Dr. Jin recommends adding a very low dosage of detoxifying herbs, such as Jin Yin Hua (Lonicerae Flos), Lian Qiao (Forsythiae Fructus), Ban Lan Gen (Isatidis/Baphicacanthis Radix), Hu Zhang (Polygoni Cuspidati Rhizoma), or Guan Zhong (Cyrtomii Rhizoma)2. For example, Isatidis root can directly inhibit the SARS coronavirus enzyme that plays a role in the replication of the virus3.
Although there is no Chinese dispensary available in St. Petersburg, there is a Cinofarm (Chinese Pharmacy) (https://cinofarm.ru/) that provides Chinese herbs in patent forms. Subsequently, it was difficult adjusting the prescription to the commercially available forms.
Herbal Prescription:
1. Mu Xiang Shun Qi Wan 8 pills x 3 times a day
Ingredients: Bing Lang Arecae semen, Chen PI (Pericarpium Citri Reticulatae), Cang Zhu (Rhizoma Atractylodis), Hou Po (Cortex Magnoliae Officinalis), Gan Cao (Radix Glycyrrhizae), Mu Xiang (Radix Aucklandiae), Sha Ren (Fructus Amomi), Sheng Jiang (Rhizoma Zingiberis Recens), Xiang Fu (Rhizoma Cyperi), Zhi Ke (Fructus Aurantii), Qing Pi (Pericarppium Citri Reticulatae Viride)
2. Xiang Sha Yang Wei Wan 8 pills x 3 times a day
Ingredients: Bai Zhu (Rhizoma Atractylodis Macrocephalae Fu Ling (Poria) Chen PI (Pericarpium Citri Reticulatae, Sha Ren (Fructus Amomi, Bai Dou Kou (Fructus Amomi Rotundus Cang Zhu (Rhizoma Atractylodis Hou Po (Cortex Magnoliae Officinalis Xiang Fu (Rhizoma Cyperi Gan Cao (Radix Glycyrrhizae) Da Zao (Fructus Ziziphi Jujibae, Guan Huo Xiang Pogostemonis/ Agastaches Herba
3. Huo Xiang Zheng Qi Wan 8 pills x 3 times a day
Ingredients: Bai Zhi Angelica dahurica, Ban Xia Pinellia Ternata, Guan Huo Xiang Pogostemonis/ Agastaches Herba, Chen PI (Pericarpium Citri Reticulatae), Da Zao Ziziphus Jujuba, Fu Ling Poria Cocos, Sheng Jiang Zingiber Officinale, Gan Cao (Radix Glycyrrhizae, Hou Po (Cortex Magnoliae Officinalis), Jie Geng, Platycodon Grandiflorus, Zi Su Ye Perilla Frutescens, Pei Lan (Eupatorii Herba), Cang Zhu (Rhizoma Atractylodis)
4. Ban Lan Gen Ke Li powder 6 g twice a day
Ingredients: Ban Lan Gen (Isatidis/Baphicacanthis Radix) Used to disperse heat-toxins from the blood level.
Analysis: Most of these available commercial herbal forms contain ingredients that are intended to release Dampness and Phlegm, promote Qi circulation, and eliminate the presence of Damp-Cold pathogens simultaneously from both the interior and superficial levels by specifically eliminating the blood toxin.
September 30th, 2020. Second online consultation.
The patient reports that his fever is still 39.4 degrees Celsius. His chills and shivering have subsided but feels cold when the temperature spikes. The patient took 1g of Tylenol to decrease the fever and feels hot once the fever goes down.
T: Red tongue with yellowish, greasy strips on sides

Pattern: Damp-Cold-Toxin in Mo Yuan, Shao Yang Pattern
Treatment: Double the dosage of previous pills and add Xiao Chai Hu Wan. Stop Ban Lan Gen Ke Li
- Mu Xiang Shun Qi Wan 16 pills x 3 times a day (increase dosage)
- Huo Xiang Zheng Qi Wan 16 pills x 3 times a day
- Xiang Sha Yang Wei Wan 16 pills x 3 times a day
- Xiao Chai Hu Tang Wan 16 pills x 3 times a day
Ingredients: Chai Hu (Radix Bupleuri|) Huang Qin (Radix Scutellariae)Dang Shen (Radix Condonopsis Pilosulae Gan Cao (Radix Glycyrrhizae)Ban Xia (Rhizoma Pinelliae, Sheng Jiang (Rhizoma Zingiberis Recens Da Zao (Fructus Ziziphi Jujibae)
Analysis: Alternating between cold and heat sensations indicates that the pathogenic dampness resides in a Shao Yang level. Xiao Chai Hu Tang is the main prescription that addresses half exterior and half interior pathogen prevalence (Shao Yang).
October 1st, 2020. 3rd consultation.
The patient presents that his fever went down to the 38.7-38.1 degrees Celsius range.
The patient was encouraged to continue the same treatment as prescribed.
October 2nd, 2020. 4th online consultation
The patient reports a fever of 37.3 degrees Celsius. His appetite is normal, and no cold or heat sensations are evidenced. The patient reports a slightly increased, non-productive cough, general fatigue, and a normal appetite. The General Blood Work results are as follows: Leukocytes 3.17 x 109/L (3.91-8.77), Neutrophiles 1.7X 109/L (1.82-7.42)
Tongue: red, swollen body, white greasy strips on side
Herbal Prescription:
- Bu Zhong Yi Qi Wan 8 pills x 3 times a day
Ingredients: Huang Qi (Radix Astragali seu Hedysari), Bai Zhu Rhizoma Atractylodis Macrocephalae), Chen PI (Pericarpium Citri Reticulatae), Ren Shen (Radix Ginseng)Zhi gan cao (Radix Glycyrrhizae preparatae), Sheng Ma (Rhizoma Cimicifugae) Chai Hu (Radix Bupleuri), Dang Gui (Radix Angelicae SinensisXiang
- Xiang Sha Liu Jun Zi Wan 8 pills x 3 times a day
Ingredients: Dang Shen (Radix Condonopsis Pilosulae, Bai Zhu (Rhizoma Atractylodis Macrocephalae, Fu Ling (Poria), Gan Cao (Radix Glycyrrhizae), Chen PI (Pericarpium Citri Reticulatae, Ban Xia (Rhizoma Pinelliae Mu Xiang (Radix Aucklandiae Sha Ren (Fructus Amomi)
- Mu Xiang Shun Qi Wan 8 pills x 3 times a day
Ingredients: Bing Lang Arecae semen, Chen PI (Pericarpium Citri Reticulatae), Cang Zhu (Rhizoma Atractylodis), Hou Po (Cortex Magnoliae Officinalis), Gan Cao (Radix Glycyrrhizae), Mu Xiang (Radix Aucklandiae), Sha Ren (Fructus Amomi), Sheng Jiang (Rhizoma Zingiberis Recens), Xiang Fu (Rhizoma Cyperi), Zhi Ke (Fructus Aurantii), Qing Pi (Pericarppium Citri Reticulatae Viride)
Analysis of formulas: The patient reports that his fever went down. His blood work shows decreased level of white blood cells. Also, his tongue still shows a greasy thick coating, indicating that the damp- toxin pathogen still persists. Furthermore, his blood count and swollen tongue body indicates that his resources, or so-called “Zhen Qi” or “Upright Qi” (the defensive mechanism that protects the body from the pathogen) has declined. Therefore, the treatment plan changed to boost his immunity and Spleen Qi and continue to eliminate the pathogen. Bu Zhong Yi Qi Tang is a formula to tonify the Spleen Qi. It is reported that Bu Zhong Yi Qi Tang can increase the number of neutrophils and accelerate recovery from cyclophosphamide-induced leukopenia in mice4. Xiang Sha Liu Jun Zi Wan tonifies Spleen Qi and eliminates Damp-Phlegm. The Mu Xiang Shun Qi Wan contains herbs that eliminate dampness from the body.
October 3rd. 2020 5th consultation.
The patient reports no fever. He feels good and was encouraged to continue the same treatment as prescribed.
October 5th. 6th consultation
The patient denies any fever. He reports a good energy and spirit. Chinese pills have created minor discomfort in his stomach, so treatment was terminated.
October 11th.
The patient’s serology test G (IgG) to SARS-CoV-2 (COVID-19) is positive. The patient feels good and returned to Canada on October 14th.
Discussion.
There were more than 300 epidemics through the history of China6. Ancient Chinese doctors, risking their own life, treated the ill using herbal medicine and documented their empirical knowledge into medical classical textbooks. Almost all were recorded and passed through the generations and were used in TCM schools. Traditional Chinese herbal medicine was effectively used during other epidemic diseases, like the Spanish flu (1918-1920)7, SARS (2002-2003)8, 2009 type A H1N1 influenza (swine flu)9, and COVID-196.
The meta-analysis of eighteen randomized controlled trials (RCTs) involving 2275 patients shows that Chinese herbal medicine increased the clinical cure rate, showed improvement on CT scans, shortened the average hospital stay, and prevented mild cases from further deteriorating into COVID-19 cases10.
In this present case, the 48-year-old male presents with symptoms of fever, chills, and radiological findings of ground-glass opacity to the right lower segment. According to the Dr. Jin Zhao, the treatment strategy should be to eliminate damp toxins from Mo Yuan (“Membrane source” – interstitial space) and disseminate the Lung Qi. Also, Huo Po Xia Ling Tang and Da Yuan Yin modifications should be utilized. Due to lack of singe herbs in Russia, the treatment was adapted to available pattern formulas. His symptoms resolved within 8 days using Chinese herbs and Tylenol only. No major side effects or complications were reported. The serology IgG test came back positive for Sars-CoV-2.
Despite the fact that Chinese medicine is very complicated, and its mechanism of the action is constantly being investigated, it is still widely used in a clinical practice. Many herbs are found to have an anti-viral activity6. One of the most significant advantages of Chinese herbal medicine is the ability to prevent complications and deterioration in mild and moderate cases6.
- Editor(s): Wei, Pei-Fang Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7), Chinese Medical Journal: May 5, 2020 – Volume 133 – Issue 9 – p 1087-1095 doi: 10.1097/CM9.0000000000000819
- Dr Jin Zhao, Chris Flanagan. Approaching covid-19 as damp toxin. The Lantern. Volume 17 No.2a Online issue March 2020 ISSN 1449-2717
- Lin CW, Tsai FJ, Tsai CH, Lai CC, Wan L, Ho TY, et al. AntiSARS coronavirus 3C-like protease effects of Isatis indigotica root and plant-derived phenolic compounds. Antiviral Res 2005; 68: 36-42.
- Kaneko M, Kawakita T, Kumazawa Y, Takimoto H, Nomoto K, Yoshikawa T. Accelerated recovery from cyclophosphamide-induced leukopenia in mice administered a Japanese ethical herbal drug, Hochu-ekki-to. Immunopharmacology. 1999 Nov;44(3):223-31. doi: 10.1016/s0162-3109(99)00050-8. PMID: 10598879.
- E-lotus institute. Coronavirus (Covid-19) and TCM: Scientific Research and ClinicalEvidence by John K. Chen, Ph.D., Pharm.D., O.M.D., L.Ac., Lori Hsu, MTOM, MS, Michael Norris, L.Ac., C.H. Debra Nash-Galpern, L.Ac. Robert Chu, OME Lorraine Wilcox, L.Ac. Donna Chow, L.Ac., DiplOM
- Lee DYW, Li QY, Liu J, Efferth T. Traditional Chinese herbal medicine at the forefront battle against COVID-19: Clinical experience and scientific basis. Phytomedicine. 2021; 80:153337. doi: 10.1016/j.phymed.2020.153337
- K.F. Cheng, P.C. Leung. What happened in China during the 1918 influenza pandemic? International Journal of Infectious Diseases, Volume 11, Issue 4,2007, Pages 360-364, ISSN 1201-9712, https://doi.org/10.1016/j.ijid.2006.07.009.
- SARS: Clinical trials on treatment using a combination of Traditional Chinese medicine and Western medicine. Report of the WHO International Expert Meeting to review and analyse clinical reports on combination treatment for SARS 8–10 October 2003 Beijing, People’s Republic of China World Health Organization. Geneva. https://apps.who.int/medicinedocs/en/d/Js6170e/4.html
- Chen W, Lim CE, Kang HJ, Liu J. Chinese herbal medicines for the treatment of type A H1N1 influenza: a systematic review of randomized controlled trials. PLoS One. 2011;6(12): e28093. doi: 10.1371/journal.pone.0028093
- Xiong X, Wang P, Su K, Cho WC, Xing Y. Chinese herbal medicine for coronavirus disease 2019: A systematic review and meta-analysis. Pharmacol Res. 2020; 160:105056. doi: 10.1016/j.phrs.2020.105056
_________________________________________________________________________________________
- Mo Yuan” (membrane source)”- space between the cells, extracellular fluid (Precision Diagnostics and Treatment Strategies in Herbal Medicine by Dr. Jin Zhao, lecture. Feb 2019. San -Diego
